In 2023, a Florida medical billing company accidentally exposed 2.7 million patient records by sending files the “wrong way”, by regular email instead of encrypted channels. They meant no harm, and were just trying to save time. But six months later, after penalties, lawsuits, and lost clients, they shut down permanently.
Every day, millions of patient records flow through medical billing systems across the country. Each claim carries deeply personal information: diagnoses that reveal private struggles, social security numbers that unlock identities, insurance details that expose financial situations. This sensitive data represents real people trusting healthcare providers with their most confidential information.
That trust rests on HIPAA compliance.
HIPAA isn't just another set of rules like any other, but the framework for ethical privacy protection in American healthcare. Followed correctly, it protects healthcare practices from devastating penalties while safeguarding the privacy patients deserve and expect.
Healthcare providers know the stakes: one wrong move with patient data can trigger devastating consequences. This guide breaks down, in a breeze, what billing teams in the US should know about HIPAA medical billing:
- Understanding HIPAA's role in billing operations
- Key compliance components and regulations
- Practical steps to avoid violations
- How modern billing services maintain compliance
- Future trends for 2026 and beyond
Whether you're new to medical billing or brushing up on existing compliance protocols, this overview will help you navigate HIPAA requirements with confidence.
Keep reading to understand why it matters for your practice in particular.
What Is HIPAA in Medical Billing?
In medical billing, The Health Insurance Portability and Accountability Act sets national standards for protecting patient health information. In medical billing, HIPAA governs how practices handle, transmit, and store patient data throughout the revenue cycle process.
HIPAA in medical billing means each interaction with patient information, from initial registration to final payment posting, must follow strict privacy and security protocols. Since their initial enrollment, these regulations have evolved to address increasing technological privacy challenges – like electronic health records, cloud storage, and remote billing operations.
Aside from obvious privacy risks, for you this matters a great deal: Violations can trigger OCR investigations resulting in penalties ranging from $100 to $2 million per violation category. Think of HIPAA as the guardrails for your billing highway; without them, patient privacy becomes impossible to protect.
Why Is HIPAA Important for Billing and Coding?
Ok, we’ve mentioned patient needs. But why is HIPAA important for billing and coding professionals? The logic is simple: Medical billing requires constant access to Protected Health Information (PHI). Every claim contains diagnoses, procedures, and personal identifiers that could expose patients to identity theft, insurance fraud, or discrimination if mishandled.
Consider this real-world example: If a billing vendor sends PHI through unsecured email to process claims faster, that single email could reasonably contain – hypothetically but reasonably – 200 patients' social security numbers, diagnoses, and insurance details. The breach could result in $1.5 million in OCR penalties, plus individual lawsuits from affected patients. That’s no joke.
Remember: Medical billing compliance protects both sides of the equation. Patients trust their information stays private. Practices avoid devastating financial penalties and reputation damage. In 2024 alone, OCR collected over $2 million in HIPAA violation settlements — and that's just the public cases.
HIPAA Meaning in Medical Billing: Key Components
Understanding HIPAA meaning in medical billing requires knowing the three core rules that govern HIPAA rules for medical billing operations:
- Privacy Rule (45 CFR Parts 164.500, 164.512, 164.520, 164.524): Establishes who can access PHI (Protected Health Information) and under what circumstances. Billing professionals can only view the minimum necessary information for their specific tasks.
- Security Rule (45 CFR Part 164, Subpart C): Mandates safeguards for ePHI (electronic Protected Health Information). This includes technical protections like encryption, physical safeguards like locked server rooms, and administrative controls like team training programs.
- Enforcement Rule (45 CFR Part 160, Subparts A and C): Sets penalty structures and investigation procedures. Fines range from $100 for unknowing infractions to $50,000+ per violation for willful neglect.
These components work together to create comprehensive protection for patient information at every touchpoint in the billing process.
How Does HIPAA Influence the Medical Billing Process?
So, how does HIPAA influence the medical billing process at each step?
Here's the complete workflow with compliance requirements:
- Patient Registration: Verify insurance through secure portals only. Never use personal email or unsecured fax. Apply the minimum necessary principle (registration personnel shouldn't see clinical notes).
- Charge Capture: Providers document services in encrypted EHR systems with unique login credentials. Automatic logoffs activate after 10 minutes of inactivity.
- Claim Submission: Billing teams transmit claims through HIPAA-compliant clearinghouses using 256-bit encryption. Each transmission creates an audit trail.
- Payment Processing: EOBs arrive through secure channels. Team members must verify recipient identity before discussing account details.
- Collections: Third-party agencies require signed Business Associate Agreements (BAAs) before accessing any PHI.
Compliant practice example: Screens face away from public areas, conversations happen behind closed doors, and documents go straight to locked shredder bins.
Non-compliant practice: Personnel discuss patient accounts in hallways, leave screens visible to waiting rooms, and toss papers in regular trash.
HIPAA Rules for Medical Billing Professionals
As mentioned, all medical billing professionals in the US work under strict HIPAA requirements that govern every aspect of their work. These rules create a framework for protecting patient information while enabling efficient billing operations.
At the core of daily operations, billing teams must follow seven essential protocols:
- Verify patient identity using two separate identifiers before releasing any billing information
- Apply the ‘minimum necessary principle’ to every data request: Only access what's needed for the specific task
- Document all PHI disclosures in detailed audit logs, including dates, reasons, and recipient information
- Complete annual HIPAA training and pass competency tests with scores of 80% or higher
- Report suspected breaches within 24 hours to designated compliance officers
- Maintain unique passwords changed every 90 days for all billing systems
- Never share login credentials between team members, even during busy periods
Beyond these daily protocols, billing professionals navigate complex authorization requirements. As such, written consent becomes mandatory before sharing billing records with anyone outside the immediate treatment team. Don’t forget this includes family members requesting statements or attorneys seeking billing documentation.
Data handling extends beyond simple access rules: Every electronic transmission requires encryption, whether sending claims to payers or payment details to patients. Audit trail documentation captures comprehensive activity logs (i.e. who accessed which records, when they viewed them, and what actions they performed). These trails prove invaluable during compliance reviews and help identify potential security breaches before they escalate.
Common HIPAA Violations in Medical Billing and How to Avoid Them
Some recent examples:
UCLA Health System paid $865,000 in fines after employees repeatedly accessed celebrity patient records without authorization. Their system lacked access controls to prevent unauthorized viewing. In another case, Advocate Health Care paid $5.5 million when four laptops containing unencrypted patient billing data were stolen from employees' vehicles
Common violations that trigger investigations:
- Emailing unencrypted patient statements to personal addresses
- Using weak passwords like "password123" for billing systems
- Discussing payment plans in waiting room areas
- Leaving printed EOBs on shared printers
- Improper disposal of paper superbills in regular trash
- Untrained personnel accessing billing systems
Prevention requires systematic approaches and constant vigilance: Install privacy screens on all monitors. Configure automatic screen locks. Implement role-based access limiting team members to only necessary functions.
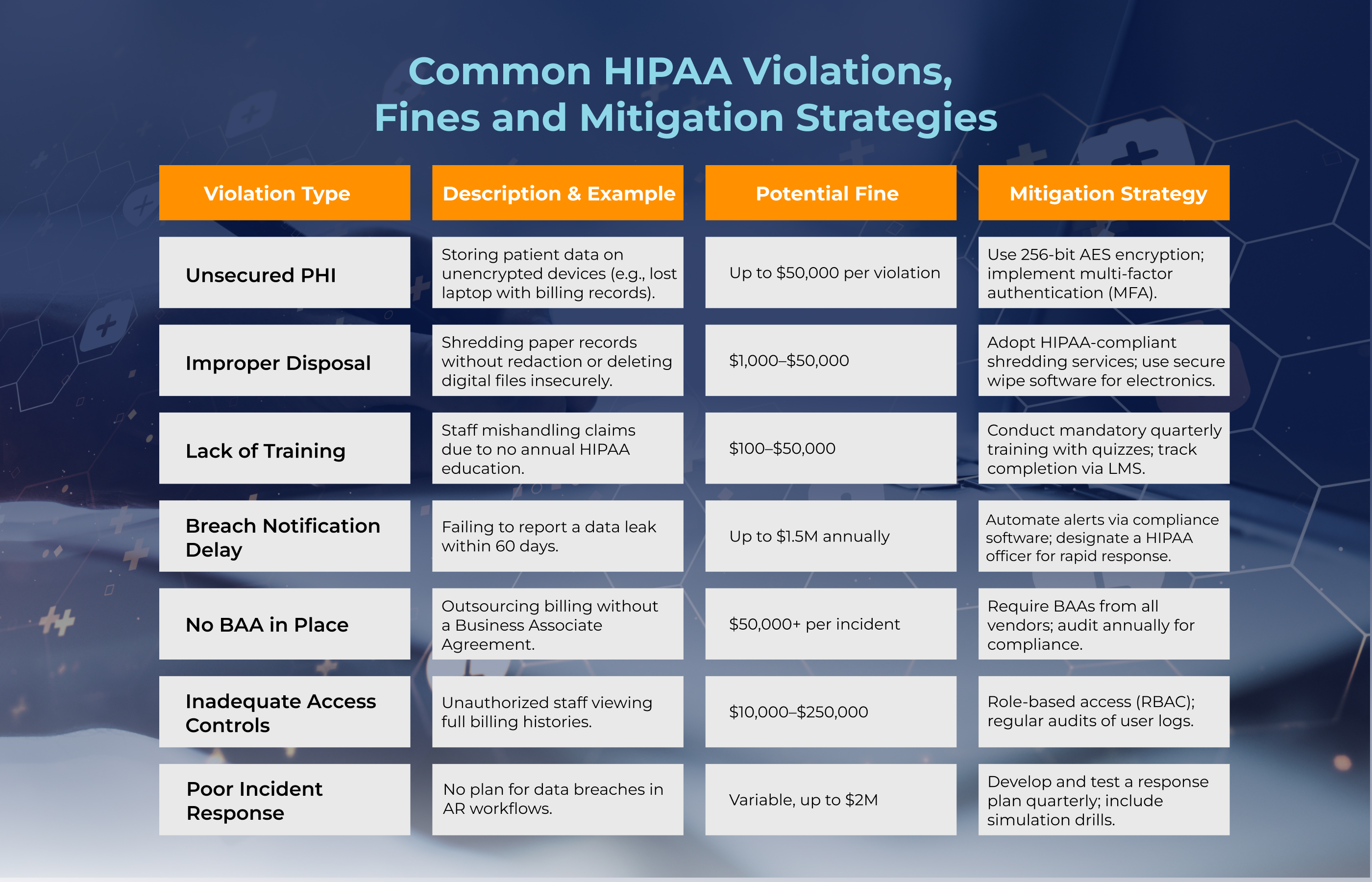
Table: Common HIPAA Violations, Fines and Mitigation Strategies
Below are examples of potential HIPAA violation costs issued by the U.S. Department of Health and Human Services (HHS) Office for Civil Rights in recent years.
For comprehensive protection, partner with medical billing services that maintain strict HIPAA compliance.
Best Practices for Achieving HIPAA Compliance in Billing Operations
It’s intimidating but true: A single breach can destroy years of reputation building. Follow these proven practices:
- Encrypt Everything: Implement 256-bit AES encryption for all ePHI transmission and storage. This includes emails, file transfers, and backup drives.
- Audit Access Monthly: Review system logs to identify unusual access patterns. Flag any after-hours access or bulk record viewing.
- Train Quarterly: Don't rely on annual training. Send monthly reminders about security protocols and test knowledge quarterly.
- Partner with Compliant Vendors: Every billing service, clearinghouse, and collection agency needs current BAAs and proof of their own compliance standards.
Consider this example case: Practice A conducts surprise audits quarterly, finding an average of 3 potential vulnerabilities before they become violations. Practice B only audits annually and suffered a $75,000 breach when a team member fell for a phishing email.
Pharmbills' Approach to HIPAA-Compliant Medical Billing
Pharmbills maintains comprehensive HIPAA compliance verified by third-party compliance provider Scytale AI Ltd. Our framework encompasses all three HIPAA rules through proven safeguards.
Privacy Rule Compliance: Pharmbills has established comprehensive policies limiting PHI use and disclosure, maintaining patient access rights, and ensuring breach notification within required timeframes (45 CFR Parts 164.500, 164.512, 164.520, 164.524).
Security Rule Implementation: We've deployed robust security measures including 256-bit encryption, role-based access controls, continuous risk assessments, and mandatory team training (45 CFR Part 164, Subpart C). Our technical safeguards include automatic session timeouts, multi-factor authentication, and encrypted data transmission channels.
Enforcement Rule Adherence: Pharmbills designated a HIPAA Privacy Officer overseeing our trained team to ensure compliance (45 CFR Part 160, Subparts A and C). We maintain detailed documentation and conduct regular audits led by Scytale to identify and address potential issues before they become violations.
Finally, Pharmbills commits to continuous improvement. We regularly review and update policies to reflect regulatory changes and industry best practices. Our team receives ongoing HIPAA training beyond minimum requirements, ensuring every billing professional understands their role in protecting patient information in billing.
The Future of HIPAA Compliance in 2026 and Beyond
HIPAA regulations in 2026 will address emerging technology challenges in medical billing: Artificial intelligence analyzing claims patterns will require new privacy frameworks. Remote billing teams accessing systems from home offices demand enhanced security protocols. Blockchain technology might revolutionize how we track PHI access and maintain audit trails, we’ll see.
By 2026, expect stricter requirements for breach notifications, potentially shrinking the window from 60 days to 24 hours. Cloud-based billing platforms will face additional scrutiny. Penalties for violations will likely increase as patient data becomes more valuable to cybercriminals.
Organizations must prepare now: The practices that stay ahead of 2026 regulations will avoid scrambling when new rules take effect. Update policies for AI tool usage in claims processing. Strengthen authentication for remote access. Plan for expanded audit requirements that could mandate real-time monitoring of all PHI access.
Final Summary
HIPAA compliance in medical billing protects the foundation of healthcare trust and patient privacy. From understanding basic requirements to implementing advanced safeguards, compliance demands expertise and constant attention. Every billing professional shares responsibility for maintaining proper compliance standards and protecting sensitive health information.
Organizations prioritizing HIPAA compliance avoid costly violations while building stronger patient relationships. The investment in proper training, technology, and partnerships pays dividends through reduced risk and enhanced reputation.
Partner with Pharmbills to ensure your billing stays fully HIPAA-compliant and efficient:



%20copy.jpeg)


