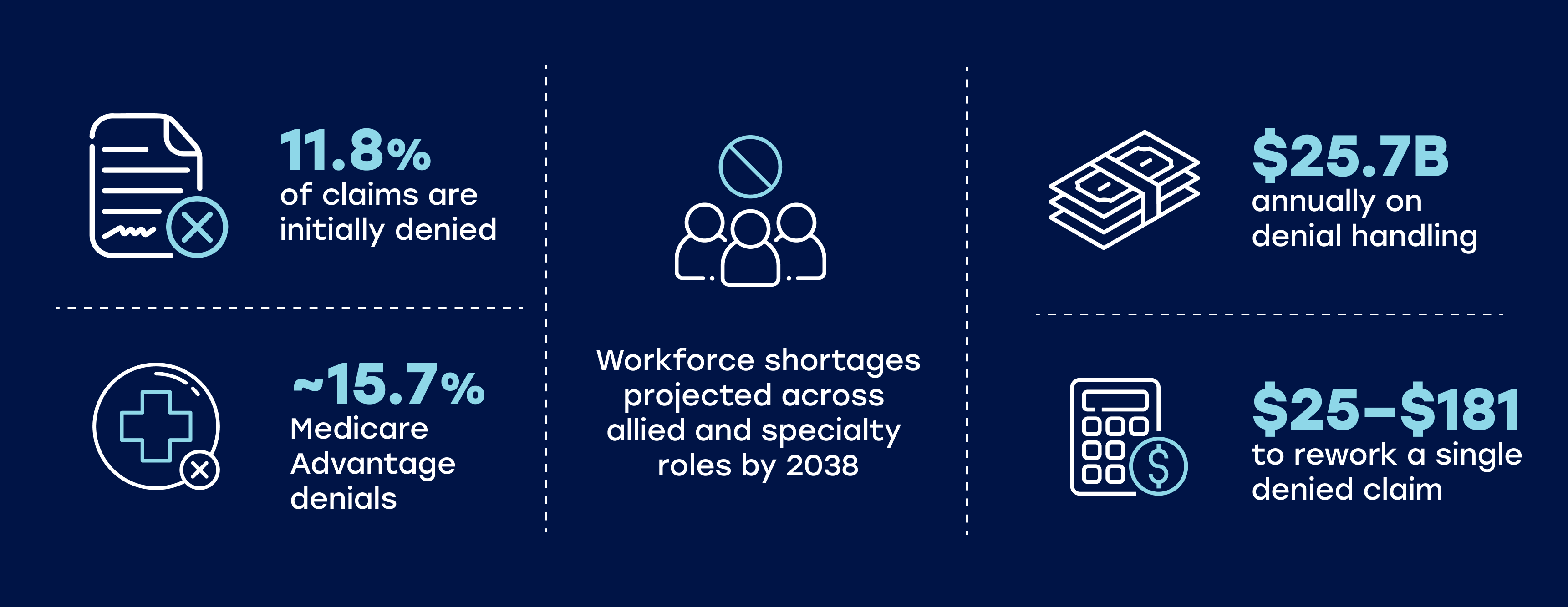
Healthcare providers face mounting financial pressures in 2026. Claim denial rates are soaring, administrative costs continue to consume 25% of healthcare spending, and health workforce shortages make in-house billing increasingly difficult. For many organizations, the support of revenue cycle management companies has become essential for maintaining healthy cash flow and sustainable margins.
Revenue cycle management (RCM) companies manage the complex flow of data and money that keeps a practice running, handling everything from patient registration and insurance verification through to coding, billing, claims, and payment collection. But in a market flooded with vendors, not all RCM partners are created equal.
In this comprehensive guide, we analyze the top revenue cycle management companies leading the market in 2026. Whether you operate a large hospital system, a specialized clinic, or a growing independent practice, this comparison guide produced by the team at Pharmbills will help you identify the partner best suited to protect your bottom line.
Related Services
Learn more about how Pharmbills supports a broad range of providers with Revenue Cycle Management Services for Healthcare.
What Is Revenue Cycle Management in Healthcare?
Healthcare revenue cycle management encompasses every administrative and clinical function that contributes to the capture, management, and collection of patient service revenue. The process begins the moment a patient schedules an appointment and continues through final payment reconciliation.
The RCM in healthcare involves managing and optimizing several interlinked stages:
- Patient intake involves collection of demographics, insurance verification (prior authorization), and eligibility checks.
- Medical coding translates clinical documentation into standardized codes, enabling accurate charge capture.
- Billing and claims management ensure accurate claims are submitted to payers and patients are promptly invoiced for any costs they are responsible for.
- Collections receives and reconciles incoming insurance and patient payments, handling denials and outstanding balances on accounts.
In 2026, more providers are turning to external healthcare revenue cycle management services to navigate the complexity involved in RCM. Partnering with one of the top rcm companies immediately benefits your organization by providing expertise across payer rules, coding updates, compliance requirements, and collection best practices.
Further Reading
For a deeper overview of this topic, read our detailed guide on What is Revenue Cycle Management (RCM) and Why Is It Important for Healthcare?
Why Choosing the Right RCM Company Matters in 2026
The healthcare financial landscape has fundamentally shifted in recent years. Three ongoing developments underpin the importance of working with only the top healthcare rcm companies.
- Surging Denial Rates
Payer complexity has intensified with new prior authorization requirements, changing reimbursement models, and stricter documentation standards. Denial rates have climbed steadily, with 41% of providers reporting denials exceeding 10% of initial submissions.
- Regulatory & Compliance Pressure
Regulatory pressure continues mounting. HIPAA enforcement has become more aggressive, with substantial fines for breaches and non-compliance. Centers for Medicare & Medicaid Services (CMS) regularly updates billing requirements, quality measures, and documentation expectations. Staying current requires constant vigilance and expertise.
- Technology-Driven RCM
Technology has transformed what's possible in revenue cycle operations. Artificial intelligence can now potentially identify coding errors before claim submission. While automation is advancing to the point of handling repetitive tasks like eligibility verification and payment posting. Advanced analytics may also predict denial patterns and suggest preventive actions.
Risk vs Reward
Partnering with the wrong healthcare RCM vendor can damage your finances through missed charges, delayed submissions, poor collections, and compliance violations.
In contrast, collaborating with the best rcm companies provides opportunities for improving cash flow, reducing denials, enhancing patient financial experience, and gaining actionable insights for operational improvements.
Overall, it’s important to remember that healthcare providers need more than basic billing services. They need partners who understand their specialty, integrate seamlessly with their practice management systems, and continuously adapt to the evolving payment landscape.
Now that we’ve covered why choosing the right RCM partner matters, let’s explore how we developed our list of the top healthcare revenue cycle management companies.
How We Selected the Top Revenue Cycle Management Companies
Selecting the top 10 rcm companies requires looking beyond marketing claims to actual performance data and client outcomes. Our evaluation framework considered multiple dimensions which are briefly described below.
Industry recognition formed a crucial baseline. The KLAS Research reports, based on thousands of provider interviews, offer perhaps the most objective assessment of vendor performance. We also examined Black Book Research rankings, HFMA awards, and Everest Group assessments to triangulate quality.
Technology capabilities matter enormously in 2026. We evaluated each company's AI and machine learning investments, their integration capabilities with major EHR systems (particularly Epic, Cerner, and athenahealth), and their approach to automation across the revenue cycle. This helped us narrow in on the top 10 healthcare RCM companies that are intelligently utilizing technology to its full capacity right now.
Specialization and scale helped us understand which providers excel in different contexts. Some top rcm companies in USA focus exclusively on large health systems, while others have built solutions specifically for ambulatory practices or specialized care settings like behavioral health and long-term care.
Client outcomes ultimately determine value. We looked for documented improvements in net revenue, days in accounts receivable, denial rates, and clean claim percentages. These are the metrics that directly impact financial performance. Above all, RCM outsourcing for medical practices must deliver tangible outcomes.
This analysis includes no paid placements or sponsored listings. Companies were selected based on market presence, documented performance, and ability to serve specific provider segments effectively. Our goal is helping you make an informed comparison rather than promoting any single vendor.
Additional Info
Before selecting an RCM partner, be sure to review these 16 Important Questions to Consider Before Choosing an RCM Vendor to ensure you evaluate all critical factors.
Comparison Table of Top RCM Companies in 2026
The following table summarizes the top 10 healthcare revenue cycle management companies serving providers in 2026, based on our comprehensive evaluation.
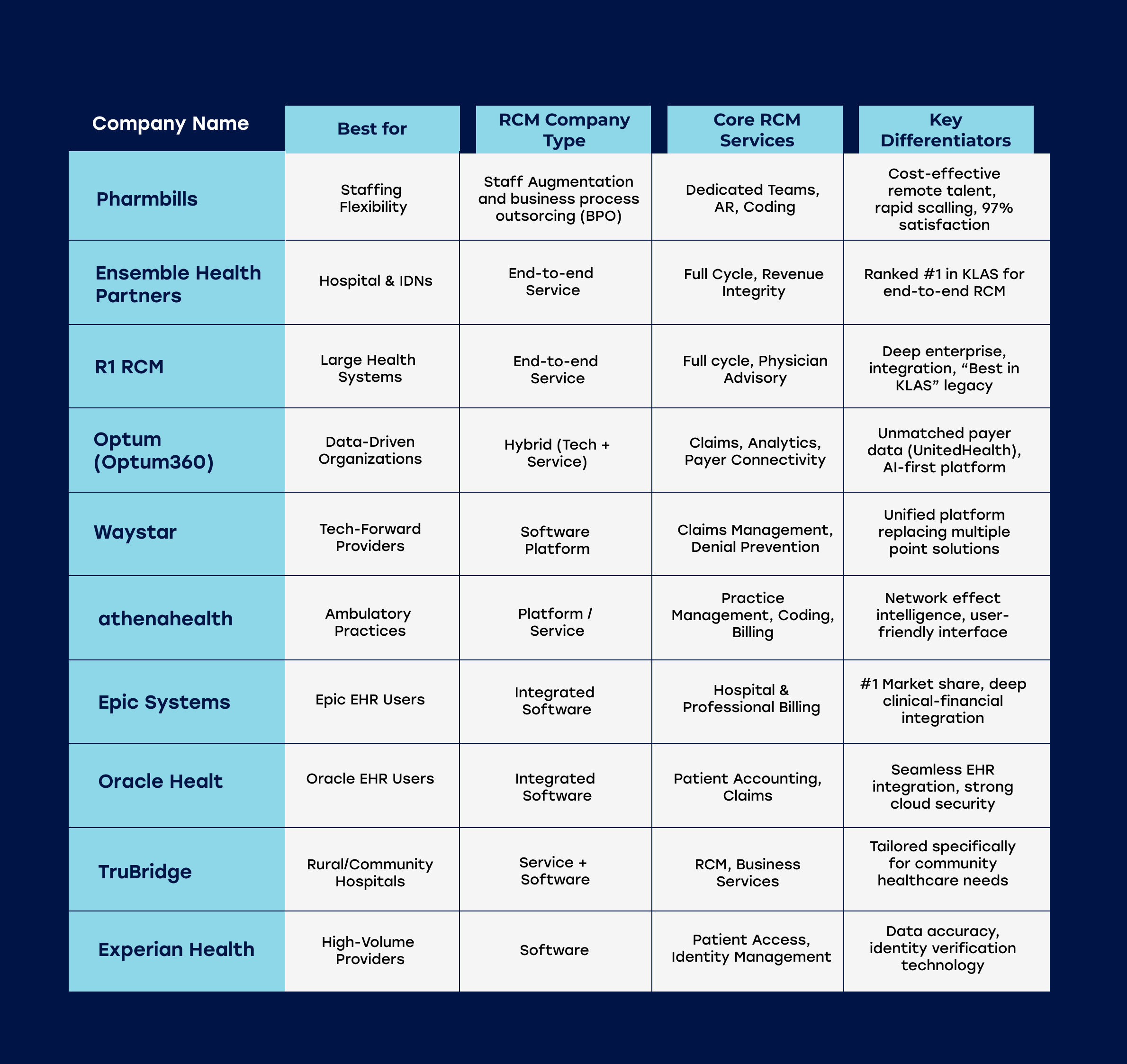
Top Revenue Cycle Management Companies for Healthcare Providers in 2026
Below are detailed profiles of our top 10 healthcare revenue cycle management companies in USA that are shaping the industry this year.
Pharmbills
Who they’re best for: Healthcare organizations of all sizes needing flexible, skilled staff augmentation to reduce labor costs without sacrificing quality.
Core services: Dedicated remote teams for A/R follow-up, medical coding, payment posting, verification of benefits, and prior authorizations.
Why Pharmbills are a top choice: While the other companies on this list sell software or total takeovers, Pharmbills solves the most immediate problem in 2026: the labor shortage. The organization provide highly skilled, English-proficient RCM talent that works directly within your existing systems (Epic, eClinicalWorks, etc.). You don't need to change your software or fire your team. Simply "plug in" Pharmbills experts to handle the time-consuming backend work, at a fraction of the cost of domestic hiring.
- Key Stat: Clients typically reduce operational labor costs by 40-50% while clearing A/R backlogs in record time.
- Pros: Zero disruption to your current workflow (no new software); rapid scaling (add 5 or 50 staff in weeks); 97% client satisfaction rate.
- Cons: Pharmbills focus on people and process. They are the ideal partner to use alongside platforms like Waystar or Epic to ensure those tools are being used effectively.
Verdict: The smartest choice for leaders who need to improve immediately while retaining control over their processes.
Ensemble Health Partners
Who they’re best for: Hospitals and Integrated Delivery Networks (IDNs) seeking a high-touch, partnership-based approach.
Core services: Ensemble offers full revenue cycle outsourcing, focusing heavily on revenue integrity and denial prevention. Unlike vendors that just process transactions, Ensemble positions itself as an operational partner that shares financial risk and reward.
Why Ensemble Health Partners are a top choice: Ensemble consistently ranks at the top of independent analyst reports (like KLAS). Their approach combines proprietary technology ("IQ") with a heavy investment in staff training. This "People + Tech" model combines AI to handle repetitive tasks and human operators for the complex denials.
- Key Stat: Ensemble claims that clients often report a 5% average lift in net patient revenue after full implementation.
- Pros: Exceptional culture and low staff turnover, leading to consistent service.
- Cons: Ensemble’s comprehensive model is designed for large-scale operations and may be "overkill" (and too expensive) for small, independent outpatient clinics.
Verdict: An excellent choice for large health systems that want an end-to-end RCM solution.
R1 RCM
Who they’re best for: Large hospital systems and physician groups looking for a complete outsourced revenue cycle management solution.
Core services: R1 RCM provides an end-to-end operating partnership model. They cover everything from patient registration to scheduling, coding, billing, and final account resolution.
Why R1 RCM are a top choice: R1 RCM has a solid reputation in the industry. Their "operating partner" model is unique because it often involves rebadging a hospital's existing RCM staff to become R1 employees. This allows them to standardize processes across massive, multi-state health systems. In 2026, their focus has shifted heavily toward automation.
- Key Stat: Claims to manage over $50 billion in Net Patient Revenue (NPR) annually.
- Pros: Huge scale and standardization capabilities; proven track record with mega-systems like Ascension and Intermountain.
- Cons: The "rebadging" process can be culturally difficult for some organizations; implementation is complex and time-consuming (6-12 months).
Verdict: Easily one of the top 10 RCM companies in USA and beyond for large systems looking for standardized, global scale.
Optum (Optum360)
Who they’re best for: Organizations that prioritize data analytics and payer connectivity.
Core services: Revenue integrity, claims management, and advanced analytics that bridge the gap between payer and provider.
Why Optum are a top choice: As a subsidiary of UnitedHealth Group, Optum possesses a dataset that other vendors struggle to match. This helps them understand exactly why payers deny claims because they are part of the same ecosystem. Their "Optum Integrity One" platform apparently utilizes this data to predict denials before a claim is even submitted.
- Key Stat: Their predictive analytics are reported to identify up to 95% of potential denials pre-submission.
- Pros: Access to one of the largest repository of claims data in the US; powerful AI tools for clinical documentation improvement (CDI).
- Cons: Some providers are hesitant to partner with a company owned by a major insurance payer, citing potential conflicts of interest. Pricing is typically geared toward the enterprise level.
Verdict: A good choice for data-driven organizations that want to leverage payer-side insights from one of the top revenue cycle management companies usa.
Waystar
Who they’re best for: Providers who want a powerful software layer to sit on top of their existing EHR/PMS.
Core services: Clearinghouse services, claim scrubbing, denial management, and patient payment estimation.
Why Waystar are a top choice: Waystar has aggressively consolidated the market, buying up niche players to create a single, unified platform for payments. Their user interface (UI) is considered one of the best in the industry. Unlike the service giants (R1/Ensemble), Waystar is primarily a technology partner. You keep your staff, but you give them Waystar to work faster and more accurately.
- Key Stat: Connects to virtually every payer in the US, reporting a 98%+ first-pass clean claim rate.
- Pros: Excellent at replacing multiple point solutions (e.g., eligibility, claims, statements) with one login.
- Cons: It is a software tool, not a service. If your internal team is understaffed or unskilled, the software alone won't fix your revenue problems.
Verdict: The best "tech stack" addition for providers who want to keep RCM services in-house but need better tools. Waystar provides RCM services for small practices and larger organizations.
athenahealth
Who they’re best for: Independent medical practices, ambulatory care centers, and provider groups.
Core services: A network-enabled platform combining EHR, practice management, and patient engagement.
Why athenahealth are a top choice: athenahealth operates on a unique "co-sourcing" model. Because their software is cloud-native, they can see denial trends across their entire network of 150,000+ providers. If a payer in Florida changes a rule, athenahealth updates its rules engine instantly, preventing that denial for every other doctor on the network. This "network intelligence" is their superpower.
- Key Stat: Their rules engine claims to contain over 40 million payer rules.
- Pros: Low barrier to entry for small practices (often taking a % of collections rather than a huge upfront fee); seamless clinical/financial integration.
- Cons: The RCM service is tightly coupled with their EHR. It is generally not a standalone solution for hospitals using Epic or Cerner.
Verdict: One of the top RCM companies in the US for independent practices wanting an all-in-one clinical and financial system.
Epic Systems
Who they’re best for: Health systems that already use the Epic EHR.
Core services: Hospital and Professional Billing modules that are fully integrated into the clinical record.
Why Epic are a top choice: Epic is among the most dominant EHRs in the US, holding the records of nearly 50% of patients. Their "Single Billing Office" approach integrates clinical and financial data into one database. This means a coder doesn't have to hunt for a doctor's note in a different system, it's all right there. This integration significantly can reduce data transfer errors and speed up billing.
- Key Stat: Regularly rated #1 for "Overall Performance" in the Best in KLAS software suite rankings.
- Pros: The "MyChart" patient portal is the gold standard for patient self-service billing; deep clinical integration reduces coding queries.
- Cons: The cost of implementation is astronomical. It is generally not an option for small practices or those not already using Epic EHR.
Verdict: If you have Epic EHR, utilizing their RCM module is often the most logical and effective choice.
Oracle Health (Cerner)
Who they’re best for: Hospitals and health systems utilizing the Oracle Health (formerly Cerner) EHR ecosystem.
Core services: Patient accounting and revenue cycle solutions focused on acute and ambulatory care.
Why Oracle are a top choice: Since Oracle's acquisition of Cerner, there has been a massive infusion of cloud technology into their RCM stack. Their new "RevElate" patient accounting solution focuses on minimizing manual touches. By automating the routine movement of data from clinical documentation to the bill, they help free up staff to work on exceptions.
- Key Stat: Oracle's cloud infrastructure claims to have some of the highest security standards in the industry, a critical factor in 2026.
- Pros: Seamless flow of data for Oracle Health clinical users; strong focus on automation and "management by exception."
- Cons: Like Epic, this is an ecosystem play. Migrating to Oracle RCM usually requires being on the Oracle EHR.
Verdict: The definitive choice for Oracle/Cerner clinical users who want to modernize their billing.
TruBridge
Who they’re best for: Rural hospitals, community healthcare centers, and critical access hospitals (CAHs).
Core services: A blend of RCM technology and business office services tailored to smaller communities.
Why TruBridge are a top choice: Rural healthcare is different. The billing rules for Critical Access Hospitals (CAHs) and Rural Health Clinics (RHCs) are unique and complex. TruBridge specializes in this niche. Their tools are built specifically for the community health market.
- Key Stat: Serves hundreds of community hospitals that are often overlooked by the "Big Box" vendors.
- Pros: Deep expertise in rural billing nuances (swing beds, cost reports); personalized service where you aren't just a number.
- Cons: They may lack the sheer scale of AI resources and big data analytics found in competitors like Optum or R1.
Verdict: TruBridge provides tailored revenue cycle optimization for healthcare providers in rural and community settings.
Experian Health
Who they’re best for: High-volume providers needing robust patient identification and front-end accuracy.
Core services: Identity management, registration QA, coverage discovery, and claims management.
Why Experian Health are a top choice: Experian isn't just a credit bureau; they are a massive player in healthcare data. They leverage their consumer data expertise to solve one of the biggest problems in RCM: patient identity. Their tools can find insurance coverage that the patient didn't even know they had ("Coverage Discovery"), recovering millions in what would otherwise be charity care.
- Key Stat: Experian’s "Coverage Discovery" tool claims to have found over $65 billion in uncompensated coverage for clients in a single year.
- Pros: Best-in-class data accuracy for patient registration; prevents front-end denials better than almost anyone else.
- Cons: Often used as a "bolt-on" solution for specific problems (like identity or eligibility) rather than a total RCM outsourcing partner.
Verdict: An essential RCM service for hospitals and health systems struggling with registration errors and uncompensated care.
Future Trends in Revenue Cycle Management (2026 and Beyond)
Four key themes are expected to shape how the top 10 revenue cycle management companies continue to evolve throughout 2026 and beyond.
- AI Billing & Predictive Analytics
Artificial intelligence is transforming coding accuracy, with AI systems now matching or exceeding human coder performance on routine cases. Predictive analytics identify claims likely to deny before submission, allowing proactive correction. Machine learning models optimize payment plan offerings based on patient financial profiles.
- Automated Prior Authorzation & Denials
Prior authorization automation is eliminating one of healthcare's most frustrating administrative burdens. Electronic prior authorization adoption continues to grow, reducing approval times from days to hours. AI systems determine when authorization is truly required versus when providers can bypass the process based on medical necessity algorithms.
- EHR and Payer Interoperability
Interoperability advances are finally delivering on long-promised seamless data exchange. FHIR standards enable real-time eligibility checks and claim status updates. Patient data flows between EHRs, billing systems, and payers without manual intervention. Clinical and financial systems increasingly operate as integrated ecosystems rather than disconnected silos.
- Increased Support for Value-Based Care
Value-based care models are fundamentally changing medical billing and revenue cycle management. RCM companies must now track quality metrics, manage risk-based contracts, and support population health initiatives alongside traditional fee-for-service billing. The top revenue cycle management companies in USA are building capabilities to manage both payment models simultaneously.
More Insights
Explore these developments further in our article on The Future of RCM: Revenue Cycle Management Trends To Watch In 2026.
Revenue Cycle Management Companies: Final Thoughts
Choosing between the top revenue cycle management companies in 2026 isn’t about finding the vendor with the flashiest AI or the biggest booth at the conference. It’s about finding the partner that fits your specific operational DNA.
Large health systems will likely be best served by end-to-end RCM outsourcing for hospitals partners like R1 or Ensemble, who can help standardize complex operations. For a tech-savvy practice, Waystar or athenahealth also offer incredible tools to modernize the front desk. And for rural providers, it’s hard to go past TruBridge. Several of the other vendors in our list of top RCM companies will suit large and small providers alike.
For organizations that want to control costs while retaining flexibility and direct oversight, a staff augmentation partner like Pharmbills offers a unique advantage. Pharmbills provides the ability to deploy expert human talent directly into your workflows, instantly solving the labor shortage problem without the disruption of a platform overhaul.
Contact Pharmbills today for a confidential discussion about how we can support your RCM and growth needs.





![Strategies for Healthcare Revenue Cycle Optimization [2026]](https://cdn.prod.website-files.com/63d9425d235def15b898f020/662b859ab4ed0e9043c16de9_21826165.jpg)
